Floaters: Possible Red-Flag Symptoms of a Serious Eye Problem by Dr Elaine Huang
If you see new floaters, they may be a sign of retinal tears or detachment.
As the name suggests, floaters are tiny specks, similar to dust that float around the field of vision. They may appear as spots, cobwebs, circles or squiggly lines and are more obvious against a bright background, such as when you are looking up into the sky or at a white computer screen. They will drift when you move your eyes and dart away when you try looking at them directly. Floaters can occur with flashes, which are perceptions of flashing lights that look like streaks of lightning or camera flashes. Rapid eye movements can aggravate the situation.
Main cause: ageing changes of vitreous gel
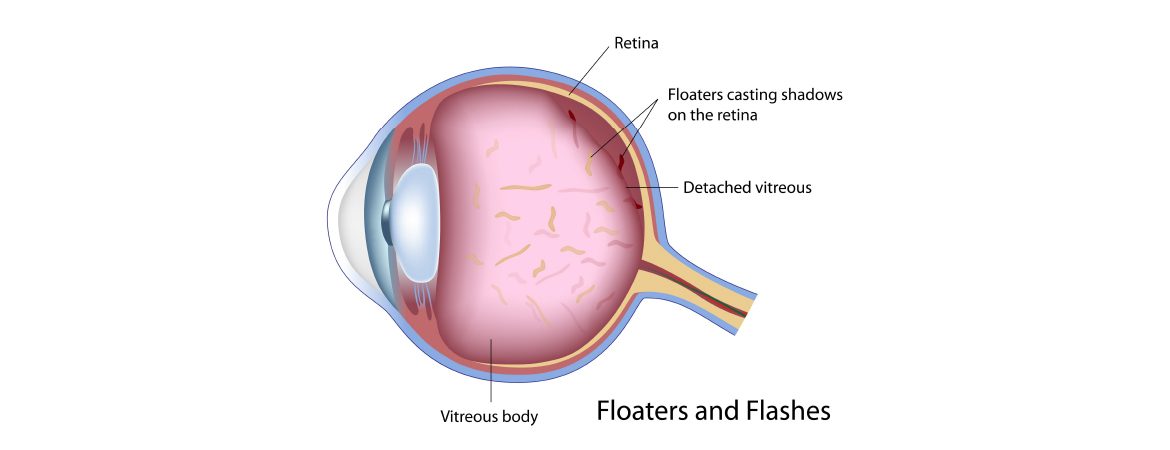
Floaters and flashes are caused by conditions associated with the vitreous, a colourless gel-like substance that fills up the space at the back of the eye.
Floaters are usually caused by age-related changes of the vitreous. As we grow older, the vitreous and its collagen fibres undergo degenerative changes, thus become stringy and opacified. Because these strands are located in front of the retina, they can cast little shadows that become more perceivable under certain lighting conditions, causing floaters.
The collapsing vitreous then pulls away from the retina as it shrinks towards the centre of the eye. This traction can stimulate the retina to cause a sensation of flashing lights. Once the gel has detached, the pulling stops and the flashes will subside.
When to worry
Even though floaters are usually benign, you should take note of the following red flags.
• A new onset or a sudden increase in floaters
• Floaters appearing immediately after flashes of light
• Associated with dark shadows in your field of vision or blurred vision
• Recent eye trauma
• High myopia
These abnormalities may indicate a possibility of retinal tears or retinal detachment.
What is retinal detachment
The retina is a thin layer of nerve tissue that lines the wall at the back of the eye. Its function is often being described as similar to the film in a camera. As rays of light pass through our pupils onto the retina, the retina transmits electrical impulses via the optic nerve to our brain. This allows our brain to interpret and make sense of the images around us.
Retinal detachment is a serious condition that occurs as a result of retinal tears. Fluid from the vitreous can enter through the tear and separate the retina from the back of the eye, causing retinal detachment. If left untreated, retinal detachment can result in permanent loss of vision.
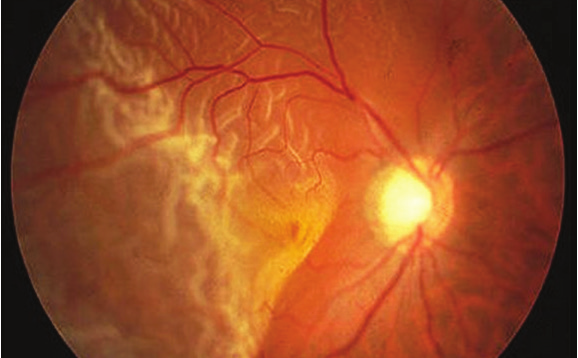
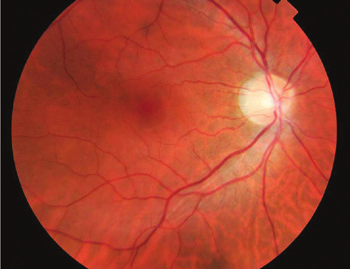
Retina detachment involving the macula (central retina)
Nonetheless, retinal tears are easily treatable by laser if they are detected early i.e. before the onset of retinal detachment. If retinal detachment occurs, surgery is usually required.
Treatment options for retinal detachment
There are different ways to treat retinal detachment.
Barrier laser photocoagulation: This can be used in a selected group of patients who have been diagnosed very early with very limited detachment.
Pneumatic retinopexy: This option is suitable for patients who have retinal breaks at the top of the retina. A gas bubble is injected into the back part of the eye to flatten out the detached retina. Laser photocoagulation is then performed to seal the breaks in the retina.
Scleral buckle: A silicone band is sutured around the sclera (white of the eye) to indent the sclera over the area where the retinal break is located. Cryopexy (freezing) is then used to seal the breaks. This band is not visible from the outside of the eye.
Vitrectomy: This involves cutting away the vitreous to relieve traction on the retina. Laser photocoagulation is also used to surround the retinal breaks. Gas is injected into the eye to tamponade the retina whilst waiting for the laser to scar and seal the breaks. There have been advances in surgical techniques, which include smaller gauge ports to gain access into the vitreous cavity, as well as ongoing improvements to 3 dimensional intraoperative visualisation. Patients will need to assume a face-down posture for two weeks after the surgery.
Risk of developing retinal detachment
For people with normal eyes, the lifetime risk of getting retinal detachment is one in every 300 people. This risk increases to one in every 20 for people with high myopia. If you have experienced retinal detachment in one eye, you have a 20% risk of experiencing the same condition in your other eye.
Treatment for floaters
If a dilated eye examination has been performed to exclude any underlying sight-threatening conditions, and your floaters are due to aging changes of the vitreous gel, you do not have to undergo any treatment.
For patients whose floaters are dense, or if the floaters are visually significant by persistently remaining in the central vision, YAG laser vitreolysis can help to reduce these visually significant floaters. This treatment involves using laser to disintegrate the opacified vitreous strands that are causing significant visual disturbance. It is painless and can be done in the clinic under topical anaesthesia using anaesthetic eye-drops. Patients may need to undergo multiple treatment sessions in order to achieve the desired outcome.
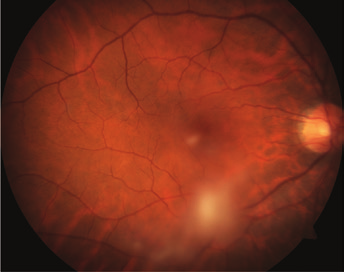
Dense blobs of opacified vitreous obscuring central vision and obstructing reading.
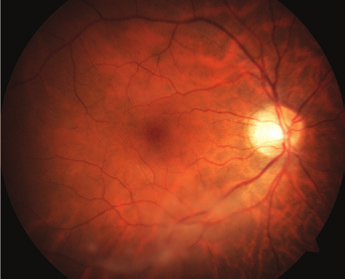
After 2 sessions of YAG laser vitreolysis: dense blobs of vitreous are significantly disintegrated.
After 4 sessions of laser treatment: resolution of central dense vitreous opacities, relieving blockage during reading.
ARTICLE ALSO WRITTEN BY DR ELAINE HUANG
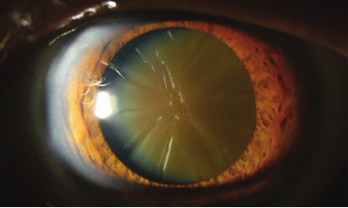
Cataracts: From Cloudy To Clear Skies

MBBS (Singapore)
MMed (Ophthalmology)
(Singapore)
MRCS (Edinburgh)
FRCS (Edinburgh)
FAMS (Ophthalmology) (Singapore) (Gold Medallist)
Dr Elaine Huang is a senior consultant ophthalmologist who specialises in managing general ophthalmology conditions, glaucoma, complicated and advanced cataract surgery. She also has subspecialised expertise in managing vitreo-retinal conditions, macular disorders, diabetic retinopathy, age-related macular degeneration, myopia and trauma-related conditions. She was formerly an Adjunct Assistant Professor at the Singapore National Eye Centre (SNEC) and Duke-NUS Graduate Medical School.
EYE MAX CENTRE
38 Irrawaddy Road
#07-42
Mount Elizabeth Novena Hospital
Singapore 329563
Tel: (65) 6694 1000 / 8181 8563
